This is a nice, clear right bundle branch block pattern: wide QRS, supraventricular rhythm (NSR), and rSR' pattern in V1. Wide little s waves in Leads I and V6 are also diagnostic. The left axis deviation indicates a left anterior fascicular block, since there is no other apparent reason for the left axis deviation, such as pathological Q waves or LVH. Left anterior fascicular block is a diagnosis of exclusion, also considering that RBBB and LAFB are often seen together (bifascicular block), since the two fascicles have the same blood supply.
Right Bundle Branch Block With Left Anterior Fascicular Block
Left Anterior Fascicular Block
This ECG provides an example of LEFT ANTERIOR FASCICULAR BLOCK (LAFB). It is from an elderly woman for whom we have no other history.
The conduction system below the AV node consists of the Bundle of His, the left bundle branch, and the right bundle branch. While there is some variation among individuals, most of us have two main fascicles, or branches, of the left bundle. The ANTERIOR-SUPERIOR fascicle carries the electrical impulse to the anterior wall of the left ventricle, and the POSTERIOR - INFERIOR fascicle carries the impulse to the inferior area of the left ventricle.
Blocks can occur at any level in the conduction system, including left bundle branch block, right bundle branch block, left anterior fascicular block, left posterior block, and bi-fascicular blocks. LAFB can have many causes, including myocardial infarction, cardiomyopathies, fibrosis of the cartilagenous ring, and aortic valve disease. Left anterior fascicular block is much more common than left posterior fascicular block. Both are also called hemiblocks.
When LAFB is present, the initial septal depolarization forces are still left to right, providing a small initial q wave in Lead I and a small r wave in Lead III. After septal depolarization is complete, the activation vector moves inferiorly and to the right as the electrical wavefront moves through the left posterior hemifascicle and right bundle branch. The impulse finally makes its way to the left and superiorly via slow conduction through myocardium normally depolarized by the left anterior hemifascicle, which is blocked. It is because the terminal left ventricular activation moves upward and toward the left that the inferior leads have negative deflections.
The diagnostic criteria for LAFB are: LEFT AXIS DEVIATION (QRS axis between -45 degrees and -90 degrees); qR pattern in Lead I; rS pattern in Lead III; delayed activation time evident in Lead aVL - the time from onset of the QRS to the peak of the R wave is 45 ms or more. (This example barely makes that criteria); QRS duration normal or slightly wide, but not 120 ms or more (unless there is also RBBB). LAFB also causes poor R wave progression in the precordial leads, with late transition and S wave present in V6.
Before deciding on a diagnosis of LAFB, you must rule out previous or acute INFERIOR WALL M.I. The pathological Q waves that can occur with necrosis can cause a left axis deviation in the frontal plane. The presence of a small r wave in Lead III rules out pathological Q wave in that lead. If any fascicular block (hemiblock or bundle branch block) occurs during the course of an M.I., the patient should be watched carefully for progression of the block. Be prepared to pace if necessary in that situation.
Thanks to our Consulting Expert, Dr. Ken Grauer, for his editing assistance.
Left Anterior Fascicular Block (Hemiblock)
This ECG provides an example of LEFT ANTERIOR FASCICULAR BLOCK (LAFB). It is from a 71-year-old woman for whom we have no other history. She also has first-degree AV block and right bundle branch block. RBBB and LAFB together are called bifascicular block. It is not uncommon to see this type of bifascicular block, as the right bundle branch and the anterior fascicle of the left bundle share a blood supply.
The conduction system below the AV node consists of the Bundle of His, the left bundle branch, and the right bundle branch. While there is some variation among individuals, most of us have two main fascicles, or branches, of the left bundle. The ANTERIOR-SUPERIOR fascicle carries the electrical impulse to the anterior wall of the left ventricle, and the POSTERIOR - INFERIOR fascicle carries the impulse to the inferior area of the left ventricle.
Blocks can occur at any level in the conduction system, including left bundle branch block, right bundle branch block, left anterior fascicular block, left posterior block, and bi-fascicular blocks. LAFB can have many causes, including myocardial infarction, cardiomyopathies, fibrosis of the cartilagenous ring, and aortic valve disease. Left anterior fascicular block is much more common than left posterior fascicular block. Both are also called hemiblocks.
When LAFB is present, the initial septal depolarization forces are still left to right, providing a small initial q wave in Lead I and a small r wave in Lead III. After septal depolarization is complete, the activation vector moves inferiorly and to the right as the electrical wavefront moves through the left posterior hemifascicle and right bundle branch. The impulse finally makes its way to the left and superiorly via slow conduction through myocardium normally depolarized by the left anterior hemifascicle, which is blocked. It is because the terminal left ventricular activation moves upward and toward the left that the inferior leads have negative deflections.
The diagnostic criteria for LAFB are: LEFT AXIS DEVIATION (QRS axis between -45 degrees and -90 degrees); qR pattern in Lead I; rS pattern in Lead III; delayed activation time evident in Lead aVL - the time from onset of the QRS to the peak of the R wave is 45 ms or more. (This example barely makes that criteria, and it is difficult to measure due to the poor copy quality); QRS duration normal or slightly wide, but not 120 ms or more (unless there is also RBBB). LAFB also causes poor R wave progression in the precordial leads, with late transition and S wave present in V6.
Before deciding on a diagnosis of LAFB, you must rule out previous or acute INFERIOR WALL M.I. The pathological Q waves that can occur with necrosis can cause a left axis deviation in the frontal plane. The presence of a small r wave in Lead III rules out pathological Q wave in that lead. If any fascicular block (hemiblock or bundle branch block) occurs during the course of an M.I., the patient should be watched carefully for progression of the block. Be prepared to pace if necessary in that situation.
For more information on hemiblocks, check Dr. Ken Grauer's ECG Blog #90 - Basic Concepts-3, and also his video on hemiblocks and axis.
Subtle ST Elevation And Left Anterior Hemiblock
We have no clinical information about this patient, except that he was complaining of chest pain, and was initially treated by prehospital paramedics.
ST Changes The paramedics noted a slight J point elevation in the precordial leads, specifically about one mm of elevation in Leads V2, V3, and V4. In addition, the ST segments are curved downward like a frown in V1 and straight in the remaining precordial leads. Because of the patient’s symptoms, and the ST abnormalities, they notified the hospital that they believed this was a STEMI. The patient was transported without complications, and the Emergency Department physician subsequently downgraded the initial assessment of STEMI Alert. We do not have access to follow up. These ST segments are abnormal, but do not necessarily indicate an acute ST-elevation M.I. (STEMI). A flat or “frowning” ST segment DOES suggest coronary artery disease, and the patient’s symptoms are worrisome. However, before activating the cath lab emergently, it is sometimes preferable to observe the patient, check cardiac enzymes and other lab results, and repeat ECGs.
Are These ST Changes Due to Acute M.I.? There are several accepted guidelines in use for evaluating ST segments for STEMI. Some are simplified for ease of use, and some are very detailed, taking into consideration the patient’s age and gender. There are ECG features that INCREASE the chances of ST elevation being due to acute M.I. These features include:
· ST elevations are in related leads
· ST segments are flat or convex upward (frowning)
· There are reciprocal ST depressions
· There are associated ECG signs of M.I. such as pathological Q waves and inverted T waves
· J points are higher than 1 mm (females have less STE requirement for M.I. diagnosis) Leads V2 and V3 generally require 2 mm of STE for a STEMI diagnosis.
As we evaluate this ECG, we see that the subtle ST elevations are in related leads (V1 - V3). They are flat (V2 and V3) or convex (V1). There is NO reciprocal depression of the ST segments. There are NO pathological Q waves. T waves are inverted in V1 and flat in Lead III, a non-specific finding. And the J points are minimally elevated at 1 mm or less. By most standard protocols, this ECG does not meet the criteria for acute STEMI. This does NOT rule out the possibility of M.I.
Other Considerations It is worth noting that strictly “normal” R wave progression is not seen in this ECG. Leads V2 through V6 show normal R wave progression. That is, the R waves progressively become proportionately larger, while the S waves regress. V1, however, does not have the morphology expected, a small r wave and a deep S wave. We are not sure if this is a lead placement issue or not. When V1 has abnormalities not shared by V2, we sometimes see similar changes in Lead III, because V1 and Lead III are both oriented toward the heart’s right side. In this ECG, Lead III does not resemble Lead V1. Also, there is a left axis deviation. If no other cause for left axis deviation is readily apparent, the cause is presumed to be LEFT ANTERIOR HEMIBLOCK, also called left anterior fascicular block. LAH is sometimes caused by anterior-septal M.I., with an incidence of about 7-15%.
Ref.:Marriott HJL, Hogan RN. Hemiblock in acute myocardial infarction. Chest.1970; 58: 342–344.
Teaching Series - Tachycardia and Left Anterior Fascicular Block
This series of three ECGs is from a 60-year-old man who was brought to the Emergency Department after being involved in a motor vehicle accident. No injuries were found, but the patient was severely intoxicated by alcohol consumption. He was conscious but agitated.
ECG NO. 1 15:07:23
The first ECG was taken by fire-rescue personnel at the scene of the accident. His hemodynamic status was stable, and the rate was not addressed in the field. ECG No. 1 shows a supraventricular rhythm at 161 bpm, with a narrow QRS and P waves visible before each QRS.
A notable feature of this ECG are the left axis deviation, by default diagnosed at left anterior hemiblock (left anterior fascicular block). The .10 second QRS width is typical of LAHB, as is the rS pattern in Lead III.
Also noted is the unusual R wave progression in the precordial leads. The R waves are prominent in V2, and then fail to progress across the precordium, and the S waves persist. This is probably due to the hemiblock. We do not know this patient’s medical history, except that he self-described as an “alcoholic”. LAFB can be associated with coronary artery disease.
ECG NO. 2 15:20:38
Now being evaluated in the Emergency Dept., we see the patient's heart rate is 163 bpm. Some variability in the rate was noted with patient agitation and activity, so it was determined that the rhythm was probably sinus tachycardia. There were no other significant changes in the ECG from the first one. Unfortunately, we no longer have access to lab results, so we do not know his electrolyte or hydration status. Labs confirmed ETOH intoxication.
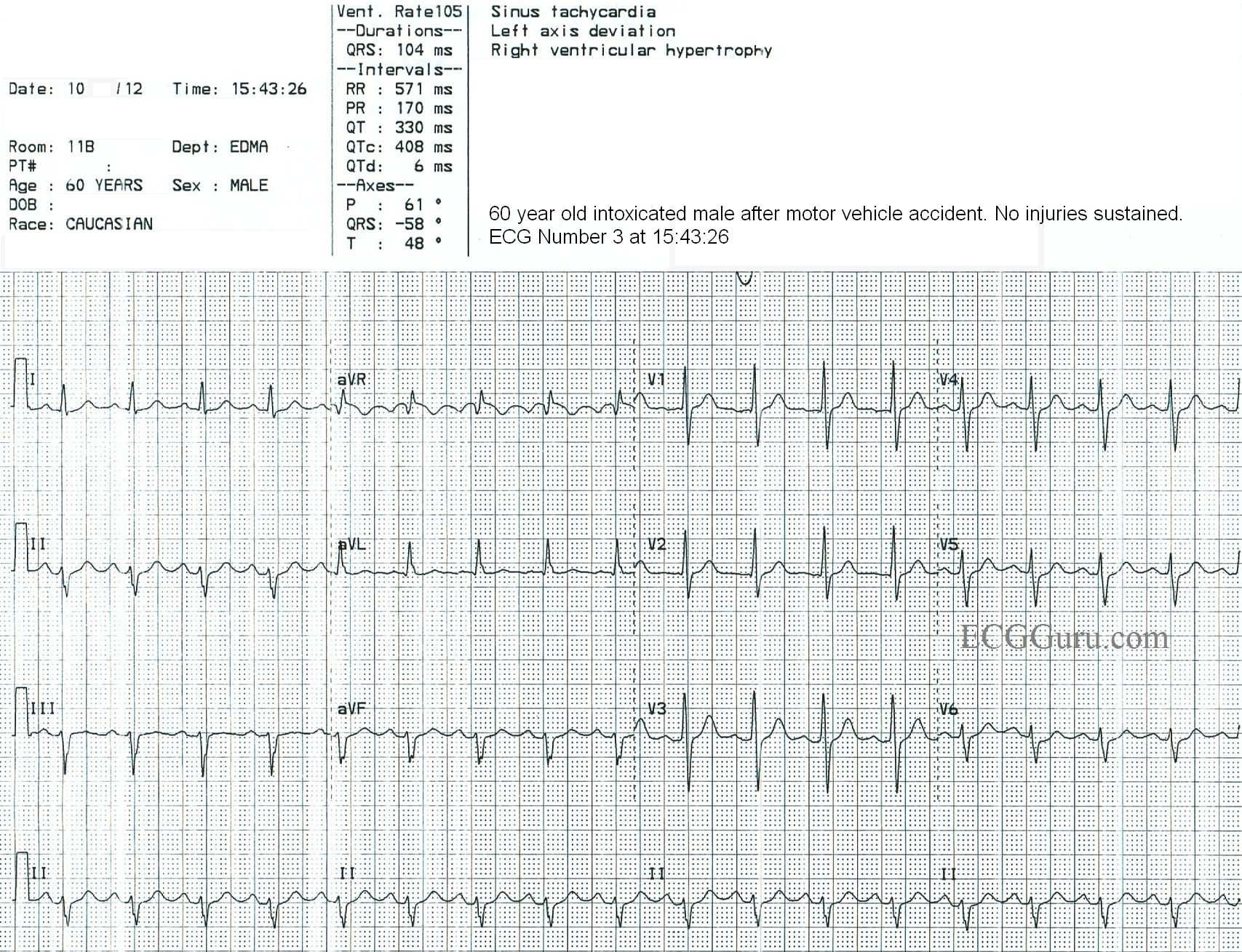
ECG NO. 3 15:43:26
After IV fluids and a short rest, the patient is much less agitated, and is conversant. His heart rate is now 105 bpm. This rate was reached by gradual increments, further evidence that this was SINUS TACHYCARDIA all along. Reentrant rhythms (AVNT, AVNRT, atrial flutter) start and stop abruptly. Some leads on ECG No. 3 may suggest an underlying atrial flutter (aVR, aVF), but the waves do not “march out”.
SINUS TACHYCARDIA VS. PSVT
At rates over 140 per minute, it can sometimes be difficult to differentiate sinus tach from reentrant tachycardias (PSVT). Seeing gradual adjustments of the rate favors a diagnosis of sinus tach. Also, seeing an obvious “cause” of sinus tach helps. In this case, the patient was a chronic alcohol abuser who was intoxicated. This is associated with sinus tachycardia, due to stimulation of catecholamine secretion and cell membrane alterations. Also, he was agitated and possibly dehydrated.
Bifascicular Block and Sinus Bradycardia
Today’s ECG is from a 75 year old man who has been experiencing syncope.
Examination of the ECG shows a sinus bradycardia at just under 40 bpm. There is a first-degree AV block, with a PR interval of about .28 seconds (280 ms). There is a right bundle branch block. The ECG criteria for right bundle branch block are: supraventricular rhythm, wide QRS (120 ms in this case), rSR’ pattern in V1, and a small, wide S wave in Leads I and V6. There is actually a “terminal delay”, or extra wave at the end of each QRS complex, reflecting late repolarization of the right ventricle.
This ECG also shows a left anterior fascicular block, also called left anterior hemiblock. The left bundle branch usually has two main branches, the anterior-superior and the posterior-inferior. ECG criteria for left anterior fascicular block are: left axis deviation with a small r wave in Lead III and a small q waves with tall R waves in Leads I and aVL. There is also a prolonged R wave peak time (> 45 ms) in aVL. There is usually a slightly prolonged QRS, but in this case, there is widening of the QRS due to the RBBB. Because the right bundle branch is blocked, and one fascicle of the left bundle is blocked, the patient is said to have a “bifascicular block”. Only one fascicle remains available for conduction from the atria to the ventricles.
We have no information about what caused the conduction block in these two fascicles, but should the third fascicle fail, the patient will be in a complete AV block. An AV block at the level of the bundle branches will result in an idioventricular escape rhythm – wide QRS complexes with very slow rates – which is a low-output rhythm.
This patient has also had syncope, which was determined to be related to his bradycardia. He had an AV sequential pacemaker implanted and did well.
Anterior Wall M.I. With Bifascicular Block
This ECG is taken from an 82-year-old man who called 911 because of chest pain. He has an unspecified “cardiac” history, but we do not know the specifics.
WHAT IS THE RHYTHM? The heart rate is 69 bpm, and there are P waves before every QRS complex. The underlying rhythm is regular, with one premature beat that is wide without a P wave. The PR interval is slightly prolonged at .25 seconds. The rhythm is normal sinus rhythm with first-degree AV block and one PVC.
WHY THE WIDE QRS? The QRS complex is wide at .14 seconds. The QRS in V 1 has a wide R wave after a small Q wave. This in consistent with right bundle branch block pattern, with loss of the normal initial small r wave (pathological Q waves). The diagnosis of RBBB is further corroborated by the wide little S waves in Leads I and V6. The QRS frontal plane axis is -66 degrees per the machine, and clearly “abnormal left” because the QRS in Lead II is negative, while the QRS in Leads I and aVL are positive. This is left anterior fascicular block, also called left anterior hemiblock. The combination of RBBB and LAFB is a common one, as the two branches have the same blood supply. It is also called bi-fascicular block.
WHAT ABOUT THE ST SEGMENTS? The ST segments in leads V2 through V6 are elevated, and their shape is very straight, as opposed to the normal shape of coved upward (smile). Even though the amount of ST elevation at the J points appears subtle, the shape of the segments, the fact that they appear in related leads, and the fact that the patient is an elderly male with chest pain all point to the diagnosis of ANTERIOR WALL ST elevation M.I. (STEMI). Additional ST changes include a straight shape in Leads I and aVL and ST depression in V1 and aVR.
PATIENT OUTCOME The patient was transported to a cardiac center, where he received angioplasty in the cath lab. The left coronary artery was found to be occluded, and was repaired and stented. He recovered without complications and was sent home in a few days.
Bifascicular Block
This ECG is from a 77 year old woman who was brought to the Emergency Department by EMS. She was found to be suffering from sepsis.
ECG Interpretation The ECG shows the expected sinus tachycardia at 123 beats per minute. There is significant baseline artifact, of the type usually seen with muscle tension. The artifact makes it difficult to assess P waves and PR intervals.
What we do see is RIGHT BUNDLE BRANCH BLOCK and LEFT ANTERIOR HEMIBLOCK, also called LEFTANTERIOR FASCICULAR BLOCK. Together, these are called BIFASCICULAR BLOCK. Most people have three main fascicles in the interventricular conduction system: the right bundle branch and the two branches of the left bundle branch, the anterior-superior fascicle and the posterior-inferior fascicle. In bifascicular block, two of the three are blocked.
The ECG criteria for right bundle branch block are:
* wide QRS (> .12 seconds)
* rSR’ pattern in V1 . (the initial R wave may be hard to see, but the QRS will be predominantly upright.
* wide little S wave in Leads I and V6.
The ECG criteria for left anterior hemiblock are:
* left axis deviation ( between -45 degrees and -90 degrees)
* small q waves in Leads I and aVL
* small r waves with deep S waves in Leads II, III, and aVF.
* delayed intrinsicoid deflection in aVL (the time between the onset of the QRS and the peak of the R wave is greater than .045 seconds).
* increased voltage in the limb leads may cause aVL to meet voltage criteria for left ventricular hypertrophy, but there will be no strain pattern.
Other causes of left axis deviation should be ruled out before diagnosing left anterior hemiblock. For example, the pathological Q waves of advanced inferior wall M.I. can cause left axis deviation, as electrical forces diminish in the damaged tissue.
Most of this ECG’s J points are at or near the baseline, with some ST depression seen in V2 through V4.
Our thanks to Jonathan Hamilton for donating this ECG
Syncope and tachycardia
The patient: This ECG is taken from a 55-year-old man whose wife called 911 because he had a syncopal episode. When the paramedics arrived, he was conscious and alert, and denied any symptoms. He gave a history of "cardiac", diabetes, and opiate abuse. We do not know the nature of his cardiac history or his medications.
It is difficult to pinpoint a definite diagnosis with this lack of information and a clearly abnormal ECG. We will limit our discussion to listing the abnormalities seen:
The ECG rhythm: There is a fast, regular rhythm that is supraventricular in origin (there are P waves). When a supraventricular rhythm has a rate of about 150 per minute, we should ALWAYS consider ATRIAL FLUTTER WITH 2:1 CONDUCTION. Atrial flutter produces P waves (flutter waves) at approximately 250-350 per minute. The normal AV node is able to conduct half of these, at a rate of about 150 per minute. Atrial flutter with 2:1 conduction is the most common presentation of new-onset atrial flutter. It is often missed by people who expect to see several flutter waves in a row, producing the "sawtooth pattern". That being said, atrial flutter is usually discernable in at least a few leads if it is present. We do not see any signs of flutter waves in this ECG.
That leaves us with a differential diagnosis of sinus tachycardia vs. one of the regular supraventricular tachycardias like reentrant tachycardias or atrial tachycardia. Sinus tachycardia can be recognized by several features. If we are fortunate enough to witness the onset or offset of the fast rhythm, will will recognize sinus tachycardia by a "warm up" or gradual speeding up of the rate, and a "cool down", or gradual slowing. On the other hand, SVTs often have abrupt onset and offset. Sinus tachycardia often has a very obvious cause, such as hypovolemia, fever, pain, anxiety, vigorous exercise, or hypoxia. Sinus tachycardia usually has a distinct, upright P wave in Lead II, and a clearly-seen, often negative, P wave in Lead V1. This ECG does not show the onset of the tachycardia, and is not long enough to evaluate for rate changes. Lead II appears to have upright P waves on the downslope of the previous T waves. V1 has deeply negative P waves, and V4 has the most clearly-seen P waves. Without being positive, this looks more like sinus tachycardia than a reentrant tachycardia. It would help to know more about the patient's condition.
The QRS complexes: The QRS complexes are slightly wide at .106 seconds. This is not wide enough to consider bundle branch block. Other conditions can cause widening, such as left ventricular hypertrophy and hemiblock, as well as some drug and electrolyte effects. The frontal plane axis is abnormally leftward, which supports a left anterior hemiblock (left anterior fascicular block) diagnosis. There is not a distinct qR pattern in Lead I or rS in Lead III, however. Lead aVF appears to have a pathological Q wave - could this be why Lead III does not have a distinct r wave?
While the chest leads do not show increased voltage that would indicate left ventricular hypertrophy, the left axis and the tall QRS in aVL do meet the criteria for LVH. LVH is not diagnosed by ECG, but it does cause changes on the ECG, such as increased voltage in left-sided leads and a "strain" pattern. Leads I and aVL demonstrate the strain pattern of downsloping ST segments and T wave inversion, but the chest leads do not.
The QRS complexes in V2, V3, and V4 are fragmented, which is an equivalent to pathological Q wave. This may indicate a prior anterior wall M.I. There is very slight J-point elevation in the right-sided chest leads, but may be due to LVH.
Without knowing more about this patient's past medical history, or the results of his physical exam, it is difficult to assign meaning to all these abnormal findings. It is unfortunate that he refused transport to a hospital, and we can only hope that he later found his way there for treatment.
Many thanks to Jon Hamilton for donating this ECG to the ECG Guru
High-grade AV Block With Bradycardia
If you are an ECG instructor, you probably carefully choose ECGs to illustrate the topic you are teaching. One of the reasons for the existence of the ECG Guru website is our desire to provide lots of such illustrations for you to choose from.
Sometimes, though, an ECG does not clearly illustrate one specific dysrhythmia well, because the interpretation of the ECG depends on so many other factors. In order to get it “right”, we would need to know information about the patient’s history, presentation, lab results, or previous ECGs. We might need to see the ECG done immediately before or after the one we are looking at. Some ECG findings must ultimately be confirmed by an electrophysiology study before we can know for sure what is going on.
For those of us who are “ECG nerds”, it can be fun to debate our opinions and even more fun to hear from wiser, more advanced practitioners about their interpretations.
My belief, as a clinical instructor, is that we must teach strategies for treating the patient who has a “controversial” ECG that take into account the level of the practitioner, the care setting, and the patient’s hemodynamic status. In some settings, it might be absolutely forbidden for a first-responder to cardiovert atrial fibrillation, for example. But atrial fib is routinely cardioverted under controlled conditions in hospitals. The general rule followed by emergency providers that “all wide-complex tachycardias are v tach until proven otherwise” has no doubt prevented deaths in situations where care providers did not agree on the origin of the tachycardia.
The ECG: We do not have much patient information to go with this ECG, just that it is from a 71-year-old woman who developed severe hypotension and lost consciousness, but was revived with transcutaneous pacing. Here is what we do know about this ECG:
· There are regular P waves, at a rate of about 39 bpm (sinus bradycardia).
· There are only two QRS complexes, shown in a total of six leads, and the rate is 13 bpm.
· The two PR intervals that are seen are the same at 368 ms, or .368 seconds (first-degree AVB).
· There are three P waves for every QRS complex. (second-degree AVB, Type II).
· The QRS complexes are 144 ms wide (.14 seconds).
· The QRS morphology cannot be evaluated in 12 leads here, but the pattern is consistent with right bundle branch block and left anterior fascicular block (bifascicular block). Were we at the bedside, another 10 seconds of 12-lead ECG might produce a QRS that falls into the remaining leads’ sections of the tracing.
It would be very important to determine what caused the severe slowing of conduction. The paper speed has not been altered, and that should be ruled out whenever all rates and intervals are prolonged. The severe sinus bradycardia, second-degree AVB, first-degree AVB, and bundle branch block all point to a global cause of poor conduction. Electrolytes, drugs, vagal stimulation, possible acute M.I. – all of these need to be assessed. And, eventually, the best definitive treatment will need to be decided.
But what is the MOST IMPORTANT issue here? The RATE! And the patient’s response to the extremely slow rate. Before we spend any time on the cause or treatment, we must address the rate and the patient’s hemodynamic status. A transcutaneous pacemaker, if available, is called for. CPR may be needed until the pacemaker can provide a perfusing rate. Rate-enhancing drugs may be used, and temporary transvenous pacing. If the patient’s perfusion status is not addressed, the rest will not matter.
When students are taking an ECG class, they most often want to know, “what is the name of this rhythm?” and “what are some shortcuts or mnemonics I can use to remember the names of the rhythms?”. They will be distressed if the instructor says, “This could be second-degree AVB, or we could call it high-grade AVB, or a longer strip might show it to be third-degree AVB.” The instructor may even feel distressed by not knowing “for sure.” But (and this is admittedly an editorial on my part), I think we do our students a disservice to lead them to believe that there is a “right” answer to every ECG strip. They need to know that some ECGs cannot and should not be read in a vacuum, but rather in light of the patient’s information. They need to know that comparison with a previous ECG, or adding additional leads, or running a longer strip may illuminate the problem. But most of all, they should understand what immediate actions can safely be taken until we do “know for sure”.
We welcome your comments on this topic, whether you are a teacher, a student, a provider, or all of these.